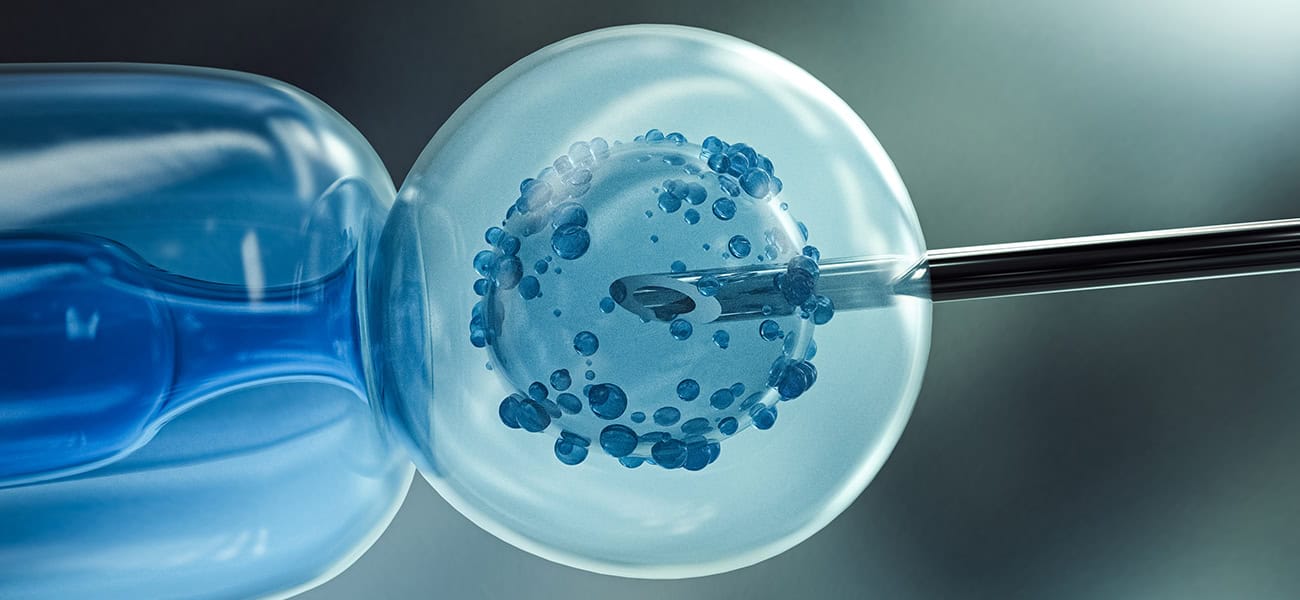
As in vitro fertilization (IVF) continues to advance, ethical considerations remain at the forefront of reproductive medicine. For professionals, navigating these complexities is critical to ensuring responsible practice and fostering trust with patients. This section explores three key ethical debates shaping the field in 2025: genetic selection, embryo storage and disposal, and equitable access to treatment. These topics reflect the evolving landscape of IVF and encourage thoughtful dialogue among practitioners.
Genetic Selection: Balancing Benefits and Risks
Preimplantation genetic testing (PGT) has revolutionized IVF by enabling the screening of embryos for genetic disorders, significantly reducing the risk of hereditary conditions. However, the use of PGT for non-medical purposes, such as selecting embryos based on physical traits, gender, or other characteristics, raises profound ethical questions. This practice, sometimes referred to as “designer babies,” prompts concerns about eugenics, societal pressures, and the potential for reinforcing biases, such as preferences for certain traits over others.
Professionals must grapple with questions about where to draw the line. Should PGT be limited to medical necessity, or is there room for patient autonomy in non-medical selections? The American Society for Reproductive Medicine (ASRM) Ethics Committee emphasizes the need for clear guidelines, noting that non-medical selection could exacerbate social inequalities and alter perceptions of human value (ASRM Ethics Committee Opinions). Practitioners are encouraged to engage in transparent discussions with patients about the implications of genetic selection, ensuring informed consent and adherence to ethical standards. This debate underscores the importance of balancing technological capabilities with societal consequences.
Embryo Storage and Disposal: Ethical Dilemmas in Cryopreservation
Advancements in cryopreservation, particularly vitrification, have made long-term embryo storage more effective, supporting fertility preservation and delayed family planning. However, this progress introduces ethical challenges regarding the management of stored embryos. What happens when patients no longer wish to use their embryos, cannot be contacted, or face disputes over ownership? Decisions about embryo disposal, donation to research, or transfer to another party are fraught with moral considerations.
For instance, some patients view embryos as potential life, complicating decisions about disposal, while others see them as medical material. Professionals must navigate these diverse perspectives while adhering to legal and ethical frameworks, which vary globally. The prolonged storage of embryos also raises practical concerns, such as storage costs and the environmental impact of maintaining cryopreservation facilities. The ASRM recommends clear policies on embryo storage duration and disposition, urging clinics to establish protocols that respect patient wishes while addressing logistical realities (ASRM Practice Committee Documents). IVF professionals should prioritize patient education and counseling to ensure clarity on these complex decisions, fostering trust and ethical integrity.
Equitable Access to IVF: Addressing Global and Local Disparities
Access to IVF remains a significant ethical concern, particularly as demand grows worldwide. The recent U.S. executive order from February 2025, aimed at expanding access and reducing costs, highlights the urgency of addressing disparities in fertility care (Expanding Access to IVF – The White House). In the U.S., many patients face barriers due to high costs and limited insurance coverage, disproportionately affecting lower-income and marginalized communities. Globally, access varies widely, with countries like Israel offering robust public funding for IVF, while others, particularly in low-resource settings, have minimal.
These disparities raise questions about fairness and justice in reproductive medicine. Should IVF be considered a universal right, or is it a privilege tied to economic and geographic factors? Professionals play a critical role in advocating for equitable access, whether through supporting policy changes, offering sliding-scale fees, or participating in global initiatives to improve fertility care infrastructure. Ethical practice demands a commitment to reducing barriers, ensuring that advancements in IVF benefit a broader population rather than perpetuating inequality.
Fostering Ethical Practice
To navigate these challenges, IVF professionals should stay informed about ethical guidelines from organizations like the ASRM and the European Society of Human Reproduction and Embryology (ESHRE). Regular training on ethical decision-making, coupled with open dialogue within clinics and the broader field, can help practitioners address these issues thoughtfully. Engaging patients in shared decision-making, grounded in transparency and empathy, is equally vital to maintaining trust and upholding ethical standards.
By addressing genetic selection, embryo storage, and equitable access, this section aims to spark reflection and discussion among IVF professionals. These ethical considerations are not only central to responsible practice but also shape the future of reproductive medicine in a rapidly evolving world.
As in vitro fertilization (IVF) continues to advance, ethical considerations remain at the forefront of reproductive medicine. For professionals, navigating these complexities is critical to ensuring responsible practice and fostering trust with patients. This section explores three key ethical debates shaping the field in 2025: genetic selection, embryo storage and disposal, and equitable access to treatment. These topics reflect the evolving landscape of IVF and encourage thoughtful dialogue among practitioners.
Genetic Selection: Balancing Benefits and Risks
Preimplantation genetic testing (PGT) has revolutionized IVF by enabling the screening of embryos for genetic disorders, significantly reducing the risk of hereditary conditions. However, the use of PGT for non-medical purposes, such as selecting embryos based on physical traits, gender, or other characteristics, raises profound ethical questions. This practice, sometimes referred to as “designer babies,” prompts concerns about eugenics, societal pressures, and the potential for reinforcing biases, such as preferences for certain traits over others.
Professionals must grapple with questions about where to draw the line. Should PGT be limited to medical necessity, or is there room for patient autonomy in non-medical selections? The American Society for Reproductive Medicine (ASRM) Ethics Committee emphasizes the need for clear guidelines, noting that non-medical selection could exacerbate social inequalities and alter perceptions of human value (ASRM Ethics Committee Opinions). Practitioners are encouraged to engage in transparent discussions with patients about the implications of genetic selection, ensuring informed consent and adherence to ethical standards. This debate underscores the importance of balancing technological capabilities with societal consequences.
Embryo Storage and Disposal: Ethical Dilemmas in Cryopreservation
Advancements in cryopreservation, particularly vitrification, have made long-term embryo storage more effective, supporting fertility preservation and delayed family planning. However, this progress introduces ethical challenges regarding the management of stored embryos. What happens when patients no longer wish to use their embryos, cannot be contacted, or face disputes over ownership? Decisions about embryo disposal, donation to research, or transfer to another party are fraught with moral considerations.
For instance, some patients view embryos as potential life, complicating decisions about disposal, while others see them as medical material. Professionals must navigate these diverse perspectives while adhering to legal and ethical frameworks, which vary globally. The prolonged storage of embryos also raises practical concerns, such as storage costs and the environmental impact of maintaining cryopreservation facilities. The ASRM recommends clear policies on embryo storage duration and disposition, urging clinics to establish protocols that respect patient wishes while addressing logistical realities (ASRM Practice Committee Documents). IVF professionals should prioritize patient education and counseling to ensure clarity on these complex decisions, fostering trust and ethical integrity.
Equitable Access to IVF: Addressing Global and Local Disparities
Access to IVF remains a significant ethical concern, particularly as demand grows worldwide. The recent U.S. executive order from February 2025, aimed at expanding access and reducing costs, highlights the urgency of addressing disparities in fertility care (Expanding Access to IVF – The White House). In the U.S., many patients face barriers due to high costs and limited insurance coverage, disproportionately affecting lower-income and marginalized communities. Globally, access varies widely, with countries like Israel offering robust public funding for IVF, while others, particularly in low-resource settings, have minimal.
These disparities raise questions about fairness and justice in reproductive medicine. Should IVF be considered a universal right, or is it a privilege tied to economic and geographic factors? Professionals play a critical role in advocating for equitable access, whether through supporting policy changes, offering sliding-scale fees, or participating in global initiatives to improve fertility care infrastructure. Ethical practice demands a commitment to reducing barriers, ensuring that advancements in IVF benefit a broader population rather than perpetuating inequality.
Fostering Ethical Practice
To navigate these challenges, IVF professionals should stay informed about ethical guidelines from organizations like the ASRM and the European Society of Human Reproduction and Embryology (ESHRE). Regular training on ethical decision-making, coupled with open dialogue within clinics and the broader field, can help practitioners address these issues thoughtfully. Engaging patients in shared decision-making, grounded in transparency and empathy, is equally vital to maintaining trust and upholding ethical standards.
By addressing genetic selection, embryo storage, and equitable access, this section aims to spark reflection and discussion among IVF professionals. These ethical considerations are not only central to responsible practice but also shape the future of reproductive medicine in a rapidly evolving world.
biweekly insights


